top of page
EDUCATIONAL ACTIVITY EXEMPLAR
Designing an Interprofessional Education Day
The College of Nursing offers a Doctor of Nursing Practice, Family & Adult Gero Acute Care Nurse Practitioner, RN-BSN, Bachelor of Science in Nursing clinical programs. As the Executive director of the Learning & Technology Resource Center (LTRC) I contribute through collaboration, management of operations, design of simulations, skills, and innovative instructional technology. One goal for our community was to incorporate IPE experiences for our learners. The largest barrier to this goal was that we were not a health science center and there were no other health professions at UAH. To initiate interprofessional education (IPE), coordination and collaboration from multiple schools who have students completing rotations within our community was necessary. With administrative support the team was able to design, implement and evaluate the first IPE day in 2017. The participating schools were: UAB School of Medicine, Auburn School of Pharmacy & UAH School of Nursing Graduate and Undergraduate programs.
In particular, the simulation scenario design was crucial in a beneficial and measurable experience for all. I followed the 11 design criteria for the standard of best practices (Lioce et.al., 2015).
-
NEEDS ASSESSMENT. Deans and directors identified a need for IPE integration into medical, nursing & pharmacy programs to role model and teach interprofessional collaboration and communication to improve patient care & safety.
-
MEASURABLE OBJECTIVES. Broad objectives were mutually agreed upon for 3 skill stations and 3 one-hour simulation cases. We identified program facilitators for each of the 6 station one from each program to provide interprofessional facilitation and feedback. The simulation broad objectives were as follows:
-
Demonstrates effective teamwork with focus on patient safety
-
Demonstrates therapeutic and confidential communication
-
Discuss & Recognize the signs and symptoms of the disease process
-
Formative documentation learning objective after each simulation
-
IPE groups collaborate to write an appropriate intervention note, assessment, and plan
-
IPE groups collaborate to write an appropriate set of orders
-
-
-
FORMAT. The IPE faculty team reserved a 7 .5 hour day for faculty and students and I designed rotation schedules.
-
SCENARIO. Three simulation cases were identified as beneficial to all participants. Simulation scenario design was initiated two months prior to the simulation activity to design roles and performance measures for all participants.
-
FIDELITY. The team reviewed and selected appropriate level modalities for the participants -partial task trainers, and high-fidelity simulators with standardized patients to increase the interaction and immersion.
-
FACILITATION. Limited patient voice cueing was allowed if guided by the well developed patient script during the scenario. Verbalization of physiologic parameters was allowed if the simulator could not display the result.
-
PRE-BRIEFING. Group pre-briefing was scripted and included all D.A.S.H. elements. The case pre-brief was led by a representative of each profession.
-
DEBRIEFING. One of the nine faculty facilitating had been trained in the Harvard method of debriefing. We chose to use the PEARLS method of debriefing and I led a training workshop and laminated handouts to support best practices.
-
EVALUATION.
-
PARTICIPANT PREPARATION.
-
TESTING - DRY-RUN.
REFERENCES
Lioce, L., Meakim, C. H., Fey, M. K., Chmil, J. V., Mariani, B., & Alinier, G. (2015). Standards of best practice: Simulation standard IX: Simulation design. Clinical Simulation in Nursing, 11(6), 309-315. http://dx.doi.org/10/1016/j.ecns.2015.03.005
Preparation
 |
|---|
 |
 |
 |
To share the vision, initial tours of the LTRC were completed with stakeholders (review preparation pictures on the left), meetings with administrations, several faculty planning sessions, facilitation & debriefing training for faculty, coordination of multi-disciplinary calendars, resources, and dates to dry-run cases with facilitators were all necessary to prepare for the experience (review planning documents on the right).
Planning

Agenda
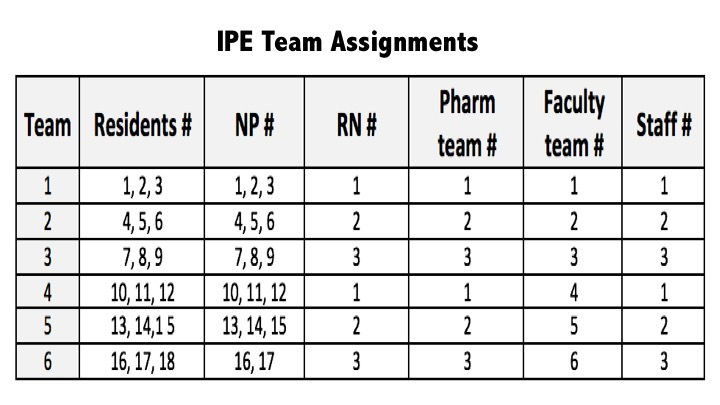
Teams

Skills

Simulation
 IPE Day June 2017 |  |  |
|---|---|---|
 |  |  |
2nd Annual Interprofessional Collaboration 2018


Flight Nursing Simulation 2018 with Mr. Bolen


Perioperative Nursing Simulation with Dr. Donna Guerra 2018

bottom of page